Human Papillomavirus (HPV) is a group of more than 200 related viruses, of which at least 14 are known to cause cancer. Among these, HPV types 16 and 18 are particularly well-documented as oncogenic, meaning they can lead to the development of various cancers, including oral cancer. Oral cancer, which affects the tissues of the mouth and throat, has been increasingly linked to HPV infection in recent years. Understanding the connection between HPV and oral cancer is crucial for awareness, early detection, and effective prevention strategies. This article delves into the relationship between HPV and oral cancer, highlighting symptoms, preventive measures, and treatment options.
What is HPV and Its Connection to Oral Cancer?
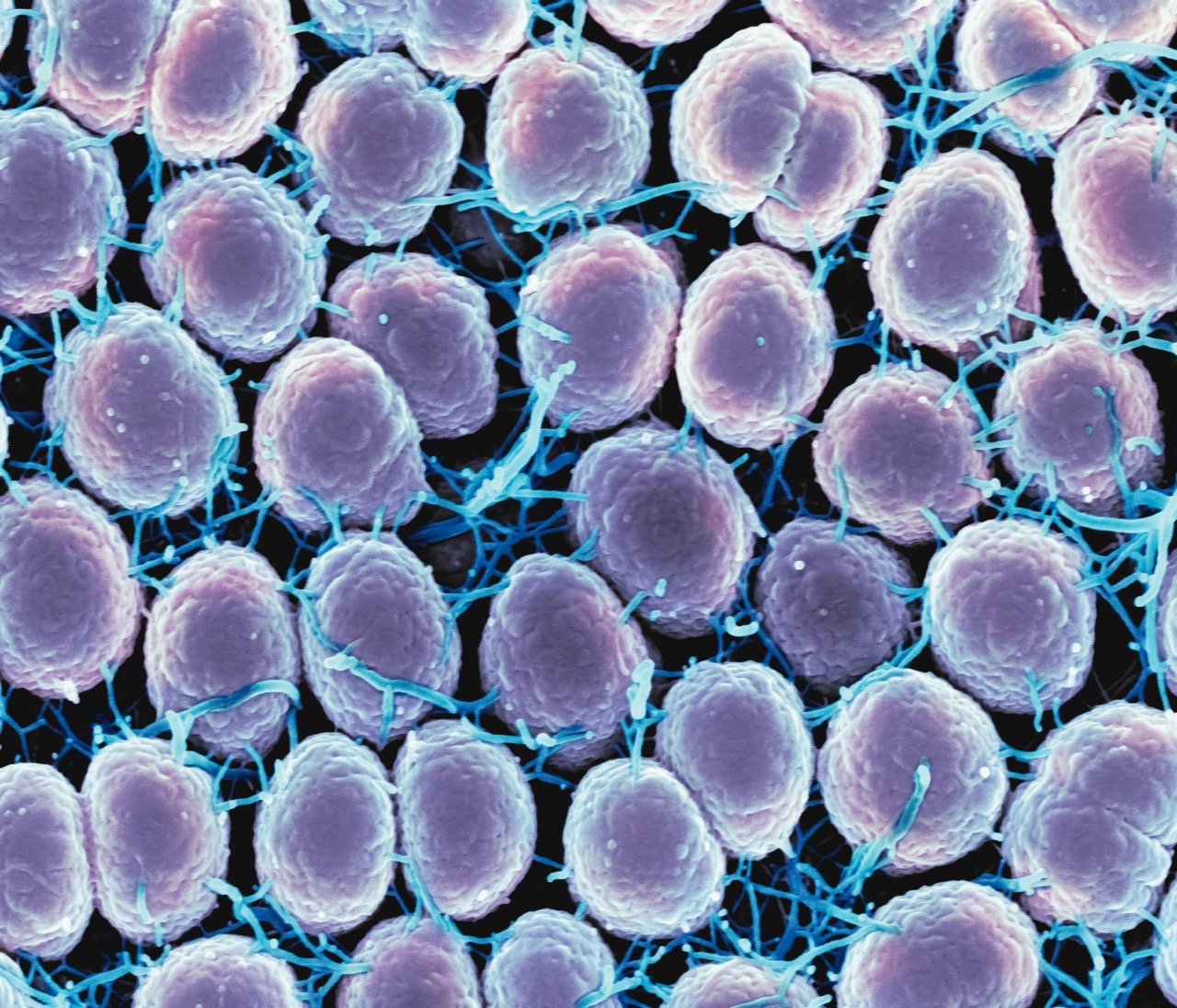
HPV is primarily known for its role in cervical cancer, but its association with oral cancers has gained significant attention in recent years. The virus is often transmitted through intimate skin-to-skin contact, including oral sex, and it can infect the mucosal surfaces of the mouth and throat. HPV-positive oral squamous cell carcinoma (OSCC) has become increasingly prevalent, particularly among younger individuals who may not have traditional risk factors such as tobacco use. Research indicates that HPV can alter the genetic structure of cells in the oral cavity, leading to malignant transformations and the development of cancer.
The pathway through which HPV leads to oral cancers involves the integration of viral DNA into the host’s cells. This can disrupt normal cell regulation, promoting uncontrolled cell growth and tumor formation. Notably, HPV-positive oral cancers often have different biological characteristics and clinical outcomes compared to HPV-negative cases. They tend to respond better to treatment and may have a better prognosis, which underscores the importance of distinguishing between these two forms of oral cancer during diagnosis and treatment planning.
Understanding the connection between HPV and oral cancer not only highlights the importance of HPV vaccination and safe sexual practices but also points to the need for ongoing research. As we learn more about the mechanisms through which HPV induces malignancy, it becomes easier to develop targeted therapies and preventive measures, ultimately improving patient outcomes.
Recognizing the Symptoms of Oral Cancer Linked to HPV
The symptoms of oral cancer can vary significantly, but those linked to HPV infection may present unique characteristics. Common symptoms include persistent sores or ulcers in the mouth, difficulty swallowing, and a change in voice. Patients with HPV-related oral cancer may also experience lumps in the neck or throat, which can indicate the spread of cancerous cells. Additionally, individuals may notice white or red patches on the mucosal surfaces of the mouth, known as leukoplakia or erythroplakia, respectively. Recognizing these signs early is crucial for timely medical intervention.
Due to the often subtle nature of symptoms, many individuals may overlook early warning signs. As HPV-related oral cancers can develop silently, it is important for individuals, especially those at higher risk, to undergo regular oral examinations. Dentists and healthcare providers play a vital role in monitoring changes in the oral cavity and can refer patients for further evaluation if suspicious lesions or symptoms are noted. Education on the symptoms associated with HPV-related oral cancer can empower patients to seek help sooner, improving the chances of successful treatment.
Moreover, awareness campaigns targeting HPV and oral cancer are essential for public health. By informing individuals about the risks, symptoms, and the importance of early detection, these initiatives can help reduce the incidence of advanced oral cancers caused by HPV. Engaging with community resources and seeking professional advice when symptoms arise can significantly impact individual health outcomes.
Preventive Measures: Reducing HPV and Oral Cancer Risks
Preventing HPV infection is the most effective strategy for reducing the risk of HPV-related oral cancer. The HPV vaccine, recommended for preteens and young adults, protects against the types of HPV that most commonly cause cancer. Vaccination can significantly reduce the incidence of HPV-related lesions and consequently lower the risk of developing oral and other HPV-associated cancers. It is essential for parents and guardians to discuss vaccination with their healthcare providers and ensure that eligible individuals receive the vaccine.
In addition to vaccination, practicing safe sexual behaviors can further reduce the risk of HPV transmission. This includes using barrier methods such as condoms and dental dams during oral sex, which can help lower the likelihood of spreading the virus. Regular screening and dental check-ups are also important preventive measures, as they allow for the early detection of any abnormal changes in the oral cavity. Individuals should be proactive in discussing their sexual health and any concerns with their healthcare providers.
Furthermore, lifestyle modifications can play a role in reducing the risk of oral cancer. Quitting tobacco use, limiting alcohol consumption, and maintaining a healthy diet rich in fruits and vegetables can bolster the immune system and enhance the body’s ability to fight infections, including HPV. Public health campaigns aimed at educating individuals about the risks associated with HPV and oral cancer can foster a culture of prevention and awareness, ultimately leading to a decrease in the incidence of these cancers.
Treatment Options for HPV-Related Oral Cancer Explained
Treatment for HPV-related oral cancer typically involves a combination of surgery, radiation therapy, and chemotherapy, depending on the stage and location of the cancer. Surgical interventions aim to remove tumor masses and affected tissues from the oral cavity. In cases where the cancer has spread to nearby lymph nodes, a neck dissection may also be necessary. The surgical approach often results in a lower recurrence rate, particularly in HPV-positive cases, which tend to respond better to treatment.
Radiation therapy is commonly used as a primary treatment or as an adjunct to surgery. It targets cancerous cells in the oral cavity and surrounding tissues, helping to eradicate any residual disease. In HPV-positive oral cancers, radiation therapy may be more effective due to the unique biological characteristics of the tumors. Chemotherapy may be employed in conjunction with radiation therapy, particularly for advanced cases where the cancer has metastasized or is aggressive in nature.
Emerging targeted therapies and immunotherapy are also showing promise in the treatment of HPV-related cancers. These therapies aim to leverage the body’s immune response to recognize and attack cancer cells. As research progresses, it is anticipated that more personalized and effective treatment options will become available, further improving outcomes for patients with HPV-related oral cancer. Ongoing clinical trials are critical for exploring new treatment avenues, and patients are encouraged to discuss potential participation in these studies with their healthcare providers.
The link between HPV and oral cancer is a growing public health concern that necessitates awareness and education. Understanding the risks associated with HPV, recognizing symptoms early, and implementing preventive measures are crucial for reducing the incidence of oral cancer. As medical research continues to evolve, so too do treatment options, offering hope and improved outcomes for those affected by HPV-related oral cancer. By prioritizing vaccination, safe sexual practices, and regular health check-ups, individuals can take proactive steps toward safeguarding their health and reducing their risk of this potentially life-threatening disease.