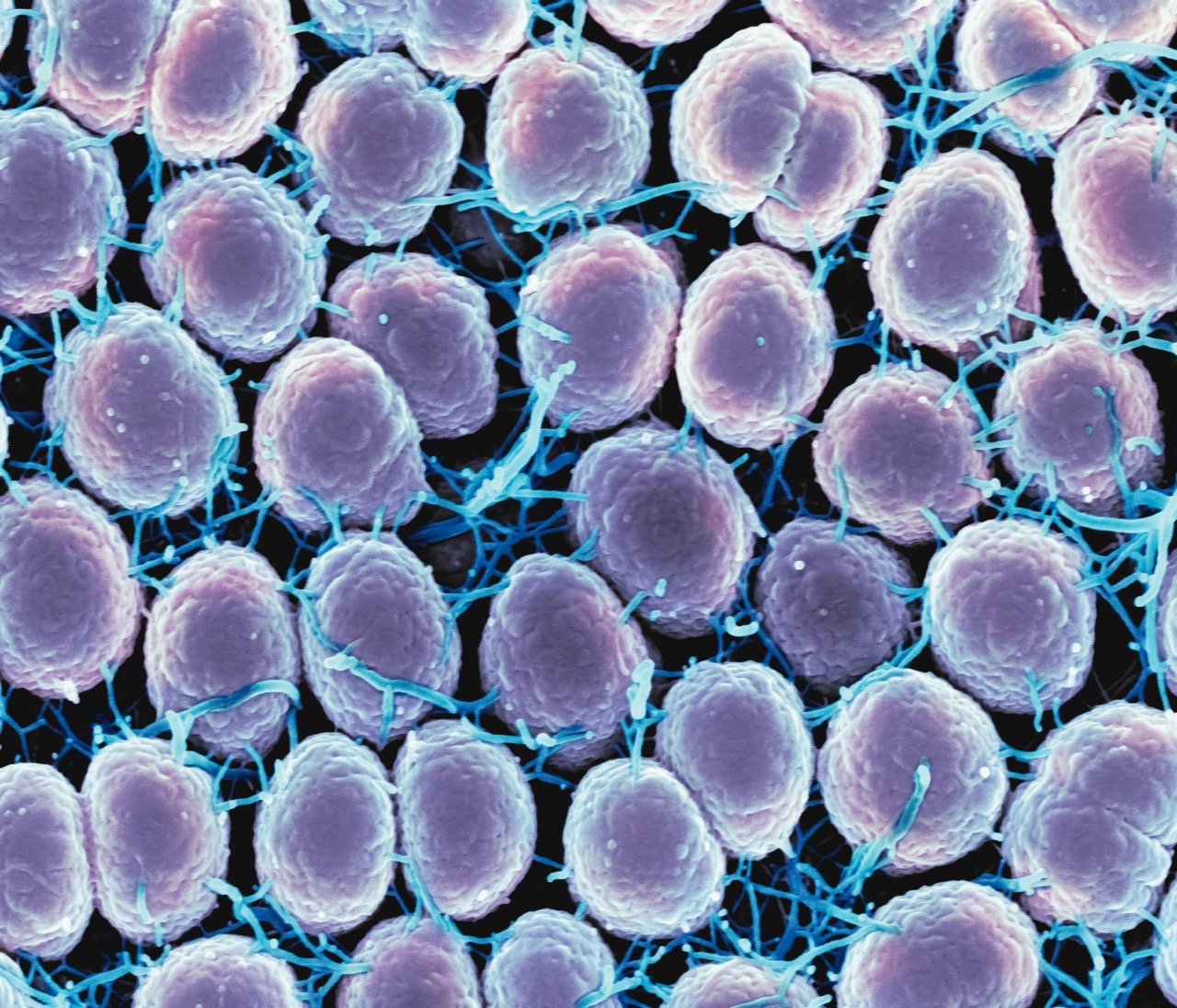
Human Papillomavirus (HPV) is one of the most common sexually transmitted infections worldwide, with numerous strains that can lead to various health issues, including genital warts and different types of cancer. To combat this public health concern, HPV vaccines have been developed and widely implemented, offering a preventative measure against several high-risk HPV strains. However, a common question arises: can you still get HPV after vaccination? Understanding the nuances surrounding HPV and its vaccination is crucial for informed health decisions.
Understanding HPV and Its Vaccination Process
HPV is a group of more than 200 related viruses, with about 40 strains that can be transmitted through intimate skin-to-skin contact. Most HPV infections do not cause symptoms and are cleared by the immune system without any long-term health implications. However, persistent infections with high-risk types can lead to cancers, particularly cervical cancer, as well as other anogenital and oropharyngeal cancers. Given the substantial burden of HPV-related diseases, the development of vaccines has been a significant milestone in public health.
There are currently three vaccines available—Gardasil, Gardasil 9, and Cervarix—each designed to protect against the most common high-risk HPV types. Vaccination is recommended for preteens, ideally around ages 11 to 12, but can be administered up to age 26 for females and age 21 for males. The vaccines are most effective when given before the onset of sexual activity, as prior exposure to HPV may reduce their efficacy. The vaccination process involves a series of two or three shots, depending on the age at initial vaccination, ensuring that individuals develop a robust immune response to the targeted strains.
Despite the effectiveness of HPV vaccines, it’s essential to recognize that they do not provide comprehensive protection against all HPV strains. While the vaccines significantly reduce the risk of infection from the most common high-risk types, there are other strains that the vaccines do not cover. Thus, individuals can still contract HPV, albeit from types not included in the vaccination regimen, emphasizing the need for ongoing education and awareness about HPV prevention.
Efficacy of HPV Vaccines Against Different Strains
Research has consistently shown that HPV vaccines are highly effective in preventing infections from the targeted strains. For example, Gardasil and Gardasil 9 are designed to protect against HPV strains 16 and 18, which are responsible for the majority of cervical cancer cases, as well as strains 6 and 11, which cause most genital warts. Gardasil 9 extends protection to five additional high-risk HPV types (31, 33, 45, 52, and 58), further enhancing its effectiveness in reducing the incidence of HPV-related diseases.
A pivotal aspect of vaccine efficacy is the population’s immunity response. Studies indicate that vaccinated individuals develop strong immunity to the targeted strains, creating herd immunity that benefits the broader community. This communal effect is crucial in reducing overall HPV prevalence and, in turn, the rates of HPV-related cancers. However, the effectiveness may wane over time, which raises discussions about the potential need for booster doses, especially for those who may have been vaccinated at a younger age.
Despite the vaccines’ efficacy, the possibility of contracting non-vaccine strains remains. The presence of numerous HPV types means that while the vaccine can significantly reduce the risk of certain strains, it does not eliminate the overall risk of HPV infection. Therefore, continued awareness about HPV transmission and safe practices is vital, even for those who have been vaccinated.
Factors Influencing HPV Infection Post-Vaccination
Several individual factors can influence the likelihood of acquiring HPV after vaccination. One critical factor is the age at which a person receives the vaccine. Vaccines are most effective when administered before the onset of sexual activity. Individuals who are already sexually active before vaccination may have been exposed to HPV strains not covered by the vaccine, increasing the risk of infection post-vaccination.
Another influential factor is the duration since vaccination. While the immunity provided by HPV vaccines is robust, it may not be lifelong. Ongoing research is needed to determine the longevity of vaccine-induced immunity and whether booster shots may be required. Additionally, individuals with compromised immune systems may not respond as effectively to the vaccine, potentially leaving them more susceptible to HPV infections.
Finally, the sexual behavior of vaccinated individuals plays a significant role in their risk of HPV infection. Engaging in unprotected sexual activities or having multiple sexual partners increases the risk of HPV exposure, regardless of vaccination status. Therefore, it’s paramount for vaccinated individuals to continue practicing safe sex and engaging in regular health screenings.
Importance of Continued Monitoring and Screening for HPV
Even with vaccination, regular monitoring and screening for HPV remains essential. The HPV vaccine significantly reduces the risk of cervical cancer; however, it does not eliminate the need for routine Pap tests and HPV screenings. These screenings are critical for detecting any abnormal cell changes in the cervix, which can lead to cancer if left untreated. Current guidelines recommend that sexually active individuals should begin cervical cancer screening at age 21, regardless of vaccination status.
Routine screening allows for early detection and the potential treatment of precancerous lesions, thus significantly lowering the risk of cervical cancer. Additionally, continued screening for HPV can help identify trends in HPV-related diseases within different populations, guiding public health initiatives and vaccination programs. This ongoing surveillance is vital for monitoring vaccine effectiveness over time and ensuring that health policies remain relevant and effective.
Moreover, continued education about HPV, its transmission, and the significance of vaccination is crucial. Misinformation or lack of awareness can lead to complacency regarding preventive measures. Engaging healthcare providers, educators, and community organizations in HPV education can empower individuals to make informed decisions about their sexual health and the importance of routine screening, regardless of vaccination.
In conclusion, while HPV vaccinations have proven to be effective in significantly reducing the risk of infection with certain high-risk strains, the possibility of contracting non-vaccine strains remains. It is essential for vaccinated individuals to understand the limitations of the vaccine and continue to engage in preventive measures such as safe sex practices and regular screenings. Ongoing education and awareness about HPV and its potential health implications will play a vital role in reducing HPV-related diseases in the long term. By prioritizing vaccination, routine monitoring, and open discussions about sexual health, individuals can take proactive steps in safeguarding their well-being.