Human Papillomavirus (HPV) is a well-known viral infection primarily recognized for its role in cervical and other anogenital cancers. Despite extensive research into its effects on reproductive health, emerging studies suggest that HPV may also be implicated in neurological symptoms. This article aims to explore the potential connections between HPV and neurological health, the current state of research in this area, and the implications for future studies and preventative measures.
Understanding Human Papillomavirus (HPV) Overview
HPV is a group of more than 200 related viruses, with over 40 types that can be transmitted through direct skin-to-skin contact, commonly during sexual activity. While many HPV infections are asymptomatic and resolve spontaneously, certain high-risk strains, particularly HPV types 16 and 18, are known to cause cancers such as cervical malignancies and oropharyngeal cancers. The virus is also associated with less common cancers, including anal and vulvar cancers. Vaccination has been developed to prevent infection by the most prevalent and high-risk strains, significantly reducing the incidence of associated cancers.
Clinically, HPV is primarily a concern for its oncogenic potential rather than other systemic effects. The virus can lead to the development of precancerous lesions, and its diagnosis typically occurs through cervical screenings or biopsies. However, the broader implications of HPV infection, including potential impacts on other organ systems, have not been thoroughly explored, leaving many gaps in our understanding of its overall health effects.
Despite the established link between HPV and various cancers, researchers are increasingly interested in understanding how the virus might influence neurological health. As the medical community begins to recognize the diverse manifestations of viral infections, it becomes essential to investigate the broader implications of HPV beyond the reproductive system. This sets the stage for exploring the potential neurological effects of the virus, a relatively uncharted territory in HPV research.
Exploring the Connection Between HPV and Neurological Symptoms
Recent investigations have begun to unravel the possible connections between HPV infection and neurological symptoms, though the evidence remains largely circumstantial and requires further validation. Some studies suggest that HPV may have a role in the development of neurological conditions like multiple sclerosis (MS) and other neuroinflammatory disorders. The hypothesis is that persistent HPV infection could trigger autoimmune responses that lead to neurological symptoms, although direct causative links have yet to be firmly established.
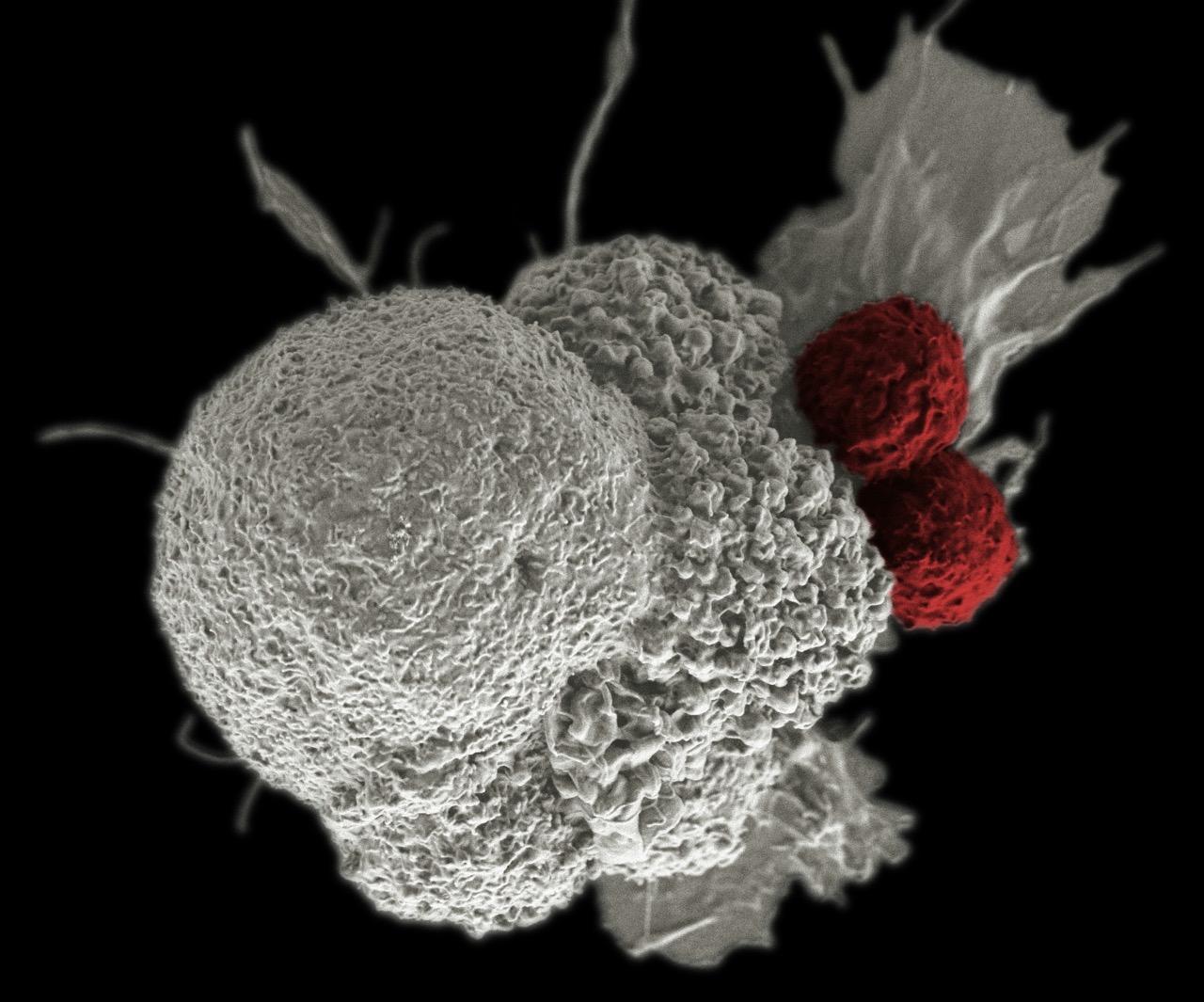
Additionally, the presence of HPV DNA has been detected in cerebrospinal fluid, indicating that the virus may have the capacity to affect the central nervous system. Some case reports have highlighted instances where patients with HPV-related cancers experienced neurological symptoms, such as cognitive impairment and peripheral neuropathy. While these observations raise important questions, they also emphasize the need for more robust, systematic studies to accurately assess the relationship between HPV and neurological manifestations.
One of the challenges in establishing causation is the multifactorial nature of neurological diseases. Conditions like MS and Alzheimer’s disease have complex etiologies that involve genetic, environmental, and infectious factors. As such, isolating HPV as a primary contributor to neurological symptoms is complicated. Nonetheless, the growing body of anecdotal evidence and preliminary studies warrants further exploration of this potential connection, as understanding this relationship may have significant implications for both HPV management and neurological health.
Current Research on HPV’s Impact on Neurological Health
Current research on HPV’s impact on neurological health is still in its infancy, with limited but promising findings emerging from various studies. Some researchers are investigating the potential mechanisms through which HPV could influence the nervous system, such as through chronic inflammation or immune-mediated pathways. These studies aim to explore how persistent HPV infections might lead to neurological issues by affecting immune responses that subsequently target the nervous system.
Moreover, researchers are also examining the prevalence of HPV in patients with specific neurological disorders. Some studies have found elevated rates of HPV infection among patients diagnosed with certain neurological conditions, indicating a possible correlation. However, such correlations do not imply causation, and more extensive epidemiological studies are essential to determine whether HPV is merely a coinciding factor or a contributing cause in these cases.
As the scientific community continues to investigate this intriguing area of research, the need for interdisciplinary collaboration is clear. Engaging virologists, neurologists, and immunologists to explore the complex interactions between HPV and neurological health could yield vital insights. This collaborative approach may help establish clearer guidelines on the screening and management of neurological symptoms in HPV-positive patients, thereby enhancing patient care and outcomes.
Preventative Measures and Future Directions in HPV Studies
Preventative measures for HPV primarily focus on vaccination, which has proven highly effective in reducing the incidence of HPV-related cancers. The introduction of the HPV vaccine has significantly lowered rates of cervical cancer and other HPV-associated malignancies. However, the potential link between HPV and neurological health highlights the importance of a more comprehensive understanding of the virus’s effects and the need for broader preventative strategies.
In addition to vaccination, public health initiatives should consider increasing awareness about the broader implications of HPV infection, including potential neurological symptoms. Educating healthcare providers and the public about the signs and symptoms of neurological disorders that may be associated with HPV could facilitate early detection and intervention. Furthermore, ongoing research efforts should be devoted to understanding the mechanisms through which HPV may impact neurological health, enabling the development of targeted therapies and management strategies.
Future studies should emphasize the need for longitudinal research that tracks HPV-positive individuals over time to assess any emerging neurological symptoms. This could involve large-scale epidemiological studies and clinical trials that examine the interplay between HPV infection and neurological health. By expanding research efforts in this area, the scientific community can generate valuable insights that enhance our understanding of HPV and potentially improve treatment options for those affected by both HPV and neurological disorders.
The potential connection between Human Papillomavirus and neurological symptoms is an emerging area of research that warrants further exploration. While current studies have opened the door to understanding how HPV might influence neurological health, much remains to be learned. As research continues to evolve, the medical community must prioritize both preventative measures and in-depth studies to understand the full scope of HPV’s effects. By advancing knowledge in this area, we can enhance patient outcomes and potentially mitigate the broader impacts of this ubiquitous virus.