Sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) are terms often used interchangeably in public discourse; however, they convey distinct meanings that are crucial for understanding sexual health. While both terms involve infections that are primarily spread through sexual contact, they differ in that STIs encompass a broader range of conditions, including those that may not yet present symptoms. This article delves into the nuances between STIs and STDs, exploring their definitions, historical contexts, epidemiological trends, and public health implications, among other facets.
Understanding STIs and STDs: Definitions and Distinctions
Sexually transmitted infections (STIs) refer to the presence of infectious agents in the body that are transmitted through sexual contact. These infections can exist without causing any symptoms, which is a significant aspect of STIs that complicates diagnosis and treatment. Conversely, sexually transmitted diseases (STDs) denote the medical conditions that arise when STIs manifest as symptoms or complications, indicating that the infection has progressed beyond an asymptomatic state. Therefore, STDs can be viewed as the clinical manifestations of infections that have significant health impacts.
This distinction is important for both healthcare professionals and the general public, as it underscores the necessity of understanding that all STDs are preceded by STIs. The terminology and understanding of STIs and STDs are not just academic; they influence public health policies, education, and individual behaviors regarding sexual health. This foundational understanding sets the stage for further exploration of the implications these differences have on prevention, diagnosis, and treatment.
Historical Context: The Evolution of Terminology in STIs
The terminology surrounding sexually transmitted infections has undergone significant evolution over the years. Initially, terms like venereal diseases (VD) were commonly used, reflecting the societal stigma associated with these infections. This term emphasized moral judgment and often led to the marginalization of affected individuals. With advances in medical understanding and a shift in societal perspectives, the term “sexually transmitted infections” emerged, aiming to reduce stigma and promote a more clinical understanding of these conditions.
The shift from VD to STIs and STDs illustrates a broader societal transformation in attitudes toward sexual health. By adopting more neutral language, public health campaigns can focus on prevention and education without the weight of moral implications. This evolution of terminology is not merely semantic; it reflects an increased awareness of the importance of sexual health as a component of overall well-being and the need for comprehensive public health strategies.
Epidemiology of STIs: Prevalence and Transmission Rates
The epidemiology of STIs reveals a concerning trend, with millions of new cases reported worldwide each year. The World Health Organization (WHO) estimates that more than one million STIs are acquired every day globally, underscoring the significant public health challenge posed by these infections. Certain demographic factors, such as age, sex, and geographic location, play critical roles in the prevalence of STIs. Young people, particularly those aged 15 to 24, are disproportionately affected, highlighting the need for targeted prevention and intervention strategies.
Transmission rates of STIs vary depending on the type of infection and the mode of sexual contact. For instance, bacterial infections such as gonorrhea and chlamydia are often transmitted through vaginal, anal, and oral sex. Viral infections, including human immunodeficiency virus (HIV), have varying transmission dynamics that can be influenced by factors such as viral load and the presence of other STIs. Understanding these epidemiological patterns is essential for developing effective public health initiatives aimed at reducing the incidence and prevalence of STIs.
Common Types of STIs: Bacterial, Viral, and Parasitic
STIs can be classified into three primary categories: bacterial, viral, and parasitic infections. Bacterial STIs include chlamydia, gonorrhea, and syphilis, all of which can be treated effectively with antibiotics if detected early. These infections, while often asymptomatic in their early stages, can lead to severe health complications if left untreated, including infertility and increased susceptibility to HIV.
Viral STIs, such as human immunodeficiency virus (HIV), herpes simplex virus (HSV), and human papillomavirus (HPV), present a different challenge. While some viral infections can be managed with antiviral medications, they often remain in the body for life and can cause long-term health issues. Parasitic STIs, including trichomoniasis, are typically less common but can cause significant discomfort and health implications. The understanding of these common types significantly informs both clinical practice and public health interventions aimed at prevention and treatment.
Symptomatology: Identifying Signs of STIs and STDs
The symptomatology associated with STIs and STDs can vary widely depending on the type of infection and the individual’s immune response. Many STIs remain asymptomatic, complicating early detection and leading to the silent spread of infections within populations. When symptoms do occur, they may include genital pain, unusual discharge, burning during urination, or sores in the genital area. The variability of symptoms necessitates regular screening for sexually active individuals, particularly those in high-risk groups.
Identifying the signs of STIs and STDs is crucial for prompt diagnosis and treatment. Some infections, like syphilis, can progress through multiple stages, each with distinct symptoms, while others may cause chronic issues if left untreated. Awareness of the symptoms associated with STIs can empower individuals to seek medical attention proactively, ultimately reducing the transmission rates and health impacts of these infections.
Diagnostic Methods: Testing for STIs and STDs Explained
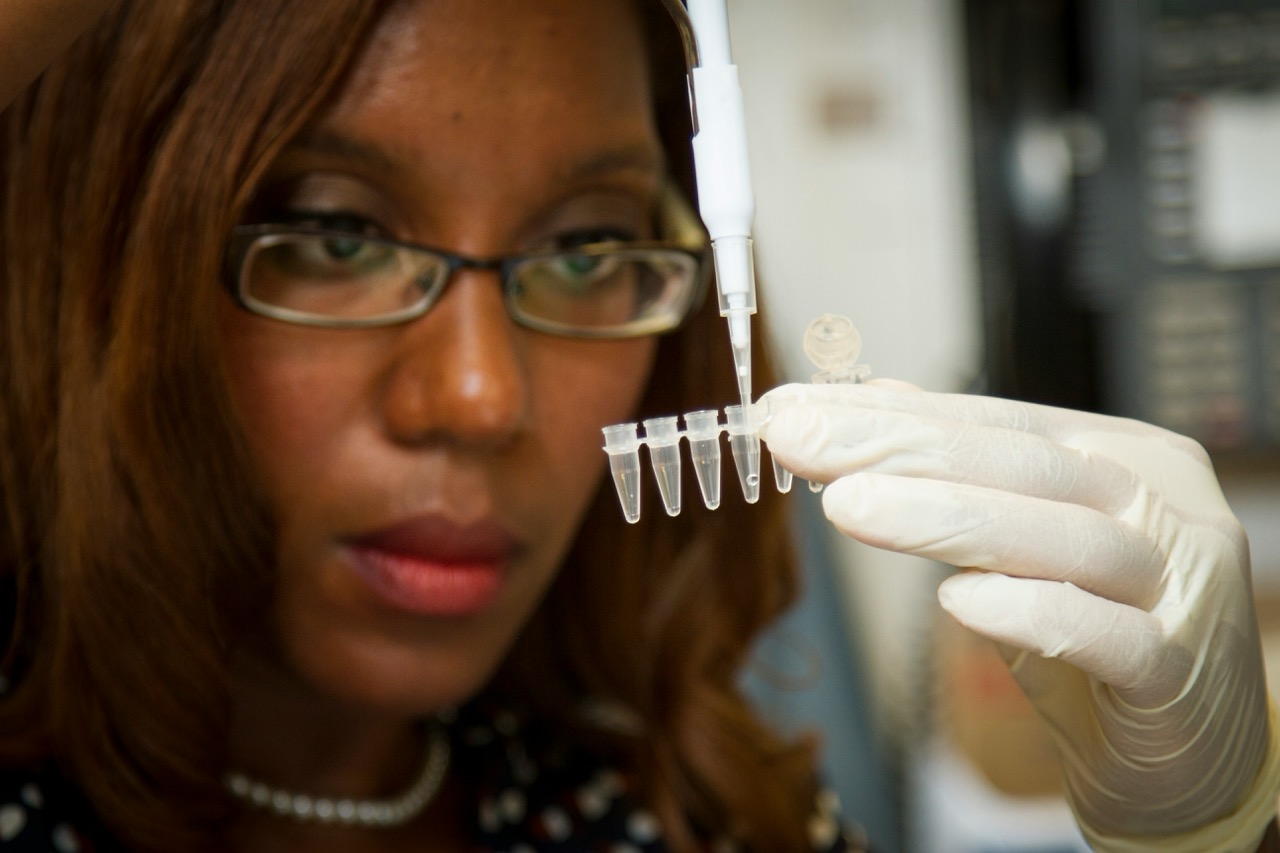
Diagnosing STIs and STDs typically involves a combination of clinical evaluation, medical history, and laboratory testing. Healthcare providers may conduct physical examinations and discuss symptoms to formulate an initial assessment. Laboratory tests, including blood tests, urine tests, and swabs from affected areas, are utilized to confirm the presence of specific infectious agents. The choice of testing method depends on the type of STI suspected and the individual’s symptoms.
Advancements in diagnostic technologies have improved the accuracy and efficiency of STI testing. Rapid test kits are now available for certain infections, allowing for quicker results and facilitating timely treatment. Moreover, the integration of routine STI screenings into general healthcare practices is essential for early detection, especially given the often asymptomatic nature of many STIs.
Treatment Protocols: Addressing STIs and STDs Effectively
Effective treatment protocols for STIs and STDs depend on the type of infection and its stage. Bacterial STIs are typically treated with antibiotics, and early intervention can lead to full recovery without long-term complications. In contrast, viral STIs require ongoing management, with antiviral medications used to control symptoms and reduce the risk of transmission. For instance, antiretroviral therapy (ART) can help individuals living with HIV maintain their health and reduce viral load to undetectable levels.
Public health guidelines delineate treatment protocols for various STIs and STDs, emphasizing the importance of both the infected individual and their sexual partners receiving treatment to prevent reinfection and further spread. Regular follow-up is also recommended to monitor treatment efficacy and address any complications. The complexities of STI management underscore the necessity of a comprehensive healthcare approach that includes education, treatment, and ongoing support.
Public Health Implications: The Burden of STIs Globally
The global burden of STIs presents significant public health challenges, with implications extending beyond individual health. High rates of STIs contribute to increased healthcare costs, lost productivity, and exacerbate existing health disparities in vulnerable populations. STIs can also facilitate the transmission of HIV and other infections, further complicating public health efforts. As such, STIs represent a critical area for intervention within global health strategies.
Addressing the burden of STIs requires coordinated efforts at multiple levels, including community engagement, policy advocacy, and resource allocation for prevention and treatment programs. Surveillance systems to track STI prevalence and incidence are essential for informing effective public health responses. Additionally, addressing the social determinants of health, such as access to healthcare and education, is vital for reducing the incidence of STIs and improving overall public health outcomes.
Prevention Strategies: Reducing Risk of STIs and STDs
Effective prevention strategies for STIs and STDs are multifaceted and encompass education, behavioral interventions, and clinical practices. Comprehensive sexual education that includes information on safe sex practices, such as condom use and regular STI testing, is fundamental to reducing transmission rates. Community outreach programs aimed at high-risk populations can further enhance awareness and accessibility to preventive measures.
Additionally, vaccination plays a crucial role in preventing specific viral STIs. For example, the HPV vaccine is effective in reducing the incidence of cervical cancer and other HPV-related diseases. Promoting regular screenings and early treatment also contributes to prevention efforts, as early detection can significantly reduce the risk of complications and transmission. Ultimately, a combination of education, access to healthcare services, and community engagement is essential for effective STI prevention.
The Role of Education: Raising Awareness on STIs
Education is a cornerstone of effective STI prevention and management. Raising awareness about STIs and STDs helps to demystify these conditions and reduce stigma associated with sexual health issues. Comprehensive sexual education programs that inform individuals about the nature of STIs, their transmission, and preventive measures are vital for fostering informed decision-making regarding sexual practices.
Moreover, public health campaigns play a crucial role in promoting awareness and encouraging individuals to seek testing and treatment. Using culturally relevant messaging and engaging community leaders can enhance outreach efforts, particularly in populations that may face barriers to accessing sexual health services. By prioritizing education and awareness, we can facilitate a more proactive approach to sexual health that empowers individuals to take charge of their well-being.
Misconceptions and Stigmas Surrounding STIs and STDs
Misconceptions and stigmas surrounding STIs and STDs contribute to significant public health challenges. Many individuals harbor beliefs that stigmatize those affected by these infections, leading to discrimination and reluctance to seek testing or treatment. Common misconceptions include the belief that only certain populations are susceptible to STIs, or that infections are a reflection of moral failing. These beliefs can hinder efforts to promote sexual health and increase the prevalence of untreated infections.
Addressing the stigma associated with STIs requires a concerted effort to reframe the narrative surrounding sexual health. Public health initiatives must focus on creating an environment where individuals feel safe to discuss their health concerns openly and seek necessary care without fear of judgment. By normalizing conversations about STIs and embracing a more compassionate approach, we can empower individuals to prioritize their sexual health and well-being.
Future Directions: Research and Innovations in STI Management
The future of STI management lies in ongoing research and innovations aimed at improving prevention, diagnosis, and treatment. Continued exploration of vaccine development for viral STIs, such as HIV and HSV, holds promise for reducing infection rates. Furthermore, advancements in diagnostic technologies, including point-of-care testing, can enhance timely detection and treatment, especially in resource-limited settings.
Additionally, research into behavioral interventions, such as the use of digital health platforms for education and outreach, may offer new avenues for engaging individuals in their sexual health. As the landscape of STIs evolves, it is essential that public health policies adapt to emerging trends and challenges, ensuring that interventions are evidence-based and culturally appropriate. Collaborative efforts among researchers, healthcare providers, and communities are vital in shaping the future of STI management.
In conclusion, understanding the differences between sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) is crucial for effectively addressing the public health challenges they present. By recognizing the importance of education, reducing stigma, and promoting awareness, individuals and communities can take proactive steps toward better sexual health. As research and innovations continue to advance, the potential for improved prevention, diagnosis, and treatment of STIs provides hope for reducing the global burden of these infections. Collaboration among healthcare providers, policymakers, and the public is essential to foster a healthier future free from the stigma and complications associated with STIs and STDs.