Sexually Transmitted Diseases (STDs) remain a critical public health issue worldwide, with millions of new infections reported annually. As treatment strategies evolve, the emergence of treatment resistance poses significant challenges to effective management. Understanding the complexities of STD treatment resistance is essential for healthcare professionals, researchers, and policymakers to develop effective interventions. This article explores the multifaceted aspects of STD treatment resistance, including underlying mechanisms, contributing factors, and implications for public health.
Overview of Sexually Transmitted Diseases and Treatment Resistance
Sexually transmitted diseases encompass a range of infections spread primarily through sexual contact. Common STDs include chlamydia, gonorrhea, syphilis, and human immunodeficiency virus (HIV). These infections can lead to severe health complications if left untreated, including infertility, chronic pain, and increased risk of acquiring or transmitting HIV. The increasing prevalence of antimicrobial resistance among these pathogens complicates treatment regimens, necessitating the exploration of alternative therapeutic options.
Treatment resistance in STDs is characterized by the failure of standard antibiotic regimens to effectively eradicate the infection. This phenomenon has escalated in recent years, primarily attributed to the overuse and misuse of antibiotics. Inadequate treatment adherence, incorrect diagnoses, and the natural evolution of pathogens further contribute to the emergence of resistant strains, highlighting the urgent need for continued vigilance and innovative strategies in STD management.
Mechanisms of Antimicrobial Resistance in STDs
The mechanisms underlying antimicrobial resistance in STDs are diverse and complex. Bacterial pathogens can acquire resistance through genetic mutations, which alter drug targets or enhance efflux pumps that expel antibiotics from the bacterial cell. Horizontal gene transfer, wherein resistant genes are exchanged between bacteria, plays a crucial role in the rapid spread of resistance among sexually transmitted pathogens.
Additionally, some STDs exhibit multi-drug resistance, complicating treatment outcomes. For instance, Neisseria gonorrhoeae, the causative agent of gonorrhea, has developed resistance to several antibiotic classes, limiting effective treatment options. Understanding these mechanisms is critical for developing targeted interventions aimed at mitigating resistance and improving treatment efficacy.
The Role of Antibiotics in STD Management
Antibiotics remain the cornerstone of STD treatment, effectively targeting bacterial infections. First-line treatments for common STDs like chlamydia and gonorrhea typically involve single-dose therapies or short-course regimens. The efficacy of these treatments hinges on the timely diagnosis and appropriate antibiotic selection, which are crucial for preventing complications and reducing transmission rates.
However, the increasing prevalence of antibiotic-resistant strains necessitates ongoing surveillance and adaptation of treatment guidelines. As resistance patterns evolve, healthcare providers must remain vigilant in reassessing the effectiveness of standard therapies and exploring alternative agents or combination therapies to ensure optimal patient outcomes.
Key Factors Contributing to Treatment Failure
Several factors contribute to treatment failure in STDs, with antimicrobial resistance being a primary concern. Misdiagnosis or delayed diagnosis can result in inappropriate or inadequate treatment, allowing resistant strains to persist and proliferate. Moreover, patient noncompliance with prescribed therapies, whether due to misunderstanding, stigma, or financial barriers, can lead to treatment failures and contribute to the spread of resistant infections.
Other contributing factors include the biological characteristics of certain STDs, such as latent infections and asymptomatic cases, which can complicate detection and treatment. The interplay of these factors underscores the need for comprehensive strategies that address both the clinical and social determinants influencing treatment outcomes.
Emerging Trends in STD Resistance Patterns
Recent studies have shown alarming trends in the emergence of resistant strains of STDs, particularly among Neisseria gonorrhoeae and Mycoplasma genitalium. Resistance to first-line antibiotics, including azithromycin and ceftriaxone, has been documented in various regions, leading to calls for revised treatment guidelines. These trends highlight the importance of monitoring resistance patterns to adapt public health responses effectively.
Furthermore, the emergence of resistant strains is not limited to bacterial STDs; viral infections, such as HIV, also demonstrate resistance to antiretroviral therapies. The increasing complexity of managing STDs in the context of resistance necessitates a multifaceted approach that includes enhanced surveillance, research into novel therapeutics, and public health awareness campaigns.
Diagnostic Challenges in Identifying Resistant Strains
Detecting resistant strains of STDs presents significant diagnostic challenges. Traditional culture methods, while effective in identifying the presence of pathogens, may not always provide timely or comprehensive information regarding resistance profiles. Rapid identification tools, such as molecular testing, are becoming increasingly important, but access to such technology can be limited in certain healthcare settings.
Additionally, the asymptomatic nature of many STDs can hinder timely diagnosis and treatment, increasing the risk of resistance development. Enhanced diagnostic capabilities are crucial for ensuring appropriate treatment decisions and minimizing the risk of treatment failure, emphasizing the need for integrated approaches that combine rapid diagnostics with effective treatment strategies.
Implications of Resistance on Public Health Strategies
The rise of treatment resistance has profound implications for public health strategies aimed at controlling the spread of STDs. As resistant strains become more prevalent, traditional treatment protocols may no longer suffice, necessitating revisions to guidelines and increased investment in research and development of new therapeutics. This challenge is compounded by the interconnectedness of global health, where resistance patterns in one region can impact public health efforts in another.
In response to these challenges, public health initiatives must prioritize education and awareness, ensuring that both healthcare providers and patients understand the importance of adherence to treatment protocols. Additionally, implementing robust surveillance systems to monitor resistance trends will be essential for informed decision-making and the allocation of resources.
Impact of Patient Noncompliance on Treatment Efficacy
Patient noncompliance is a significant barrier to successful STD treatment and can exacerbate the problem of treatment resistance. Failure to complete prescribed antibiotic regimens or attend follow-up appointments can lead to treatment failures, facilitating the persistence and spread of resistant strains. Factors influencing noncompliance include socioeconomic status, lack of understanding of the infection, and stigma associated with STDs.
Addressing patient noncompliance requires a multifaceted approach, involving education, counseling, and support services. Healthcare providers must create an open and nonjudgmental environment, encouraging patients to discuss their concerns and challenges. By fostering a collaborative relationship, providers can improve treatment adherence and ultimately enhance outcomes in the management of STDs.
Advances in Molecular Testing for Resistant STDs
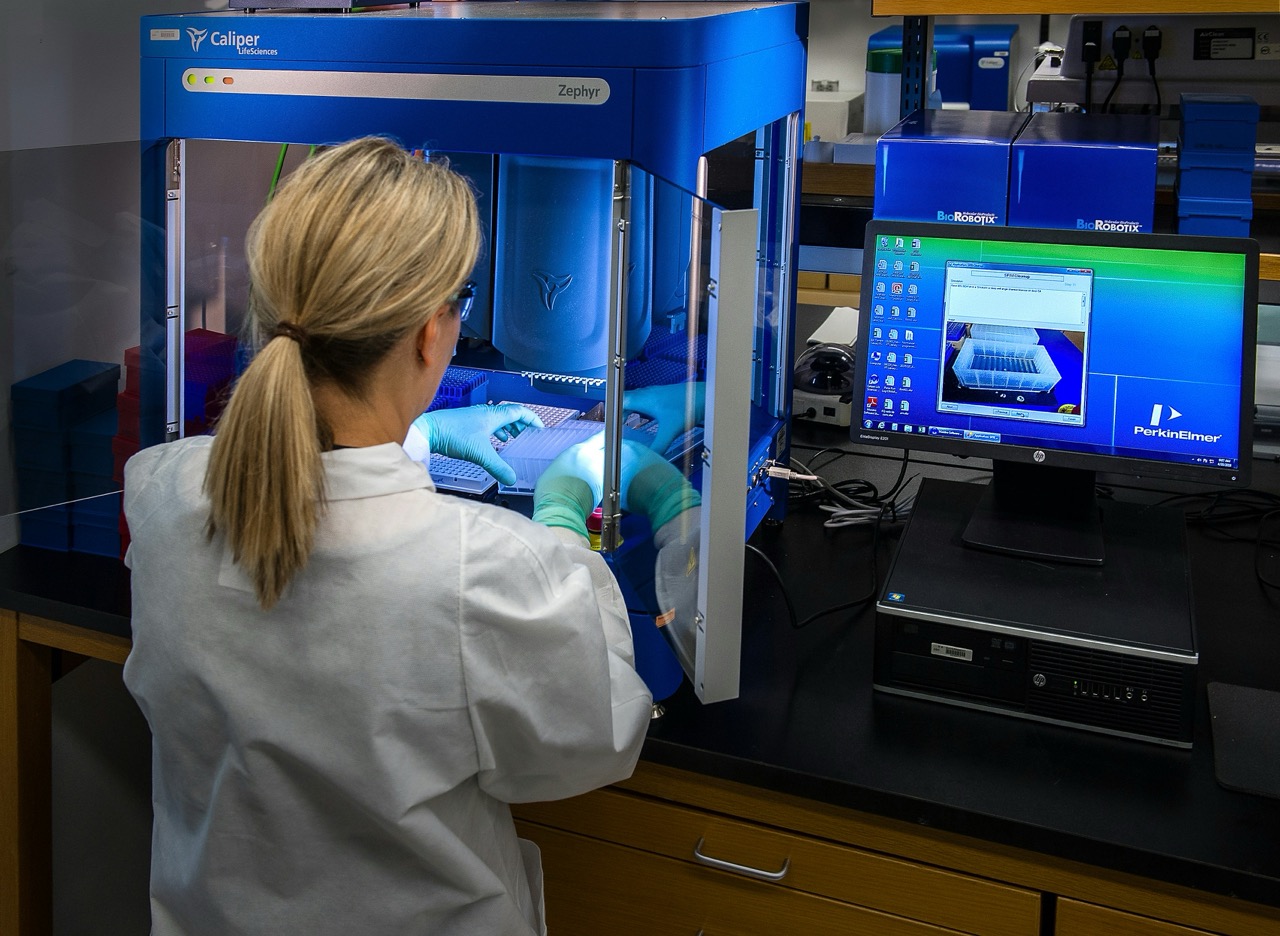
Recent advances in molecular testing technologies have revolutionized the detection and characterization of resistant STDs. Techniques such as polymerase chain reaction (PCR) and next-generation sequencing allow for rapid identification of pathogens and their resistance profiles, providing clinicians with critical information for tailoring treatment. These innovations enable the detection of resistant strains that may not be identifiable through traditional methods, making them invaluable in combatting treatment resistance.
Moreover, molecular testing facilitates the early identification of outbreaks and emerging resistance patterns, allowing public health officials to implement timely interventions. The integration of these advanced diagnostic tools into routine clinical practice is essential for enhancing the effectiveness of STD management and mitigating the impact of treatment resistance.
Strategies for Overcoming Treatment Resistance in STDs
Addressing treatment resistance in STDs requires a multifaceted approach that includes judicious use of antibiotics, improved diagnostic capabilities, and patient education. Healthcare providers must be vigilant in prescribing antibiotics only when necessary and ensuring that patients understand the importance of adherence to prescribed regimens. Developing alternative treatment strategies, such as combination therapies, may also be crucial in overcoming resistance.
Public health campaigns aimed at raising awareness about STDs and promoting safe sexual practices can help reduce transmission rates and the development of resistant strains. Additionally, fostering collaboration between healthcare providers, researchers, and policymakers will be vital in developing comprehensive strategies to combat treatment resistance effectively.
The Importance of Surveillance in STD Resistance
Surveillance is a critical component in the fight against STD treatment resistance. By systematically monitoring resistance patterns, public health officials can identify emerging threats and implement targeted interventions. Surveillance data can inform treatment guidelines, facilitating timely revisions based on the evolving landscape of resistance.
Furthermore, robust surveillance systems can enhance the understanding of the epidemiology of STDs, allowing for the identification of high-risk populations and the allocation of resources where they are needed most. The integration of surveillance data with clinical practices will be essential for developing effective public health strategies that address the complexities of treatment resistance.
Future Directions for Research and Treatment Approaches
Research into new treatment modalities and strategies for managing resistant STDs is essential for addressing the growing public health crisis. Investigating alternative antibiotics, vaccine development, and innovative therapeutic approaches, such as bacteriophage therapy, may provide new avenues for combating resistant strains. Additionally, ongoing research into the mechanisms of resistance will be vital for developing targeted interventions.
Collaboration between researchers, healthcare providers, and public health officials will be crucial in driving innovation and translating research findings into clinical practice. Investment in research initiatives and funding for studies focused on resistant STDs will help pave the way for more effective treatment options and improved patient outcomes in the future.
The emergence of treatment resistance in sexually transmitted diseases poses significant challenges for healthcare providers and public health systems. Understanding the underlying mechanisms, contributing factors, and implications of resistance is crucial for developing effective strategies to combat this issue. Continuous advancements in diagnostic capabilities and treatments, combined with robust surveillance systems and patient education, are essential to ensure effective management of STDs in an era of rising resistance. Addressing this public health challenge requires a collaborative and comprehensive approach that prioritizes research, innovation, and the well-being of individuals at risk for STDs.